What is FUE?
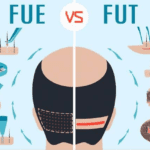
Follicular Unit Excision, also known as FUE (previously Follicular Unit Extraction) is another widely-used and popular harvesting method. The other being “FUT” or the “strip” harvesting techniques. FUE is a technique that uses tiny tools to remove follicular units “one by one” from the donor area. This is different from strip, which involves removing a small piece of hair-bearing tissue from the donor. A doctor performing FUE carefully “scores” each follicular unit within the donor area using circular “punch”, or 1.2mm diameter tools. Then, the doctor uses forceps (tweezers), to pull or pluck the unit from the skin. The tiny hole left by the procedure is allowed to heal and becomes a “dot scar.” FUE does not require staples or sutures. The FUT procedure involves the extraction of grafts and refinement.
FUE is not like the strip technique. It leaves no incision scars in the donor area. It leaves thousands of tiny “dots” scars from the graft removal. This scarring is less noticeable in the right patient, and can be worn with shorter hairstyles in the back if done correctly. There is no “scarless” hair transplant procedure. FUE can cause visible scarring if the donor area has been trimmed sufficiently. Although estimates vary, most patients can trim to about a #2 (fourth inch of hair) before FUE scarring becomes visible. FUT patients typically can reduce to a #3 (3/8 of an in) before the linear scar becomes visible. FUE must use a larger area of donor hair to avoid over harvesting and creating thin patches. FUE must also be performed on the back of the head, which is different from FUT, where the hair is left long. This can make concealing your procedure during the post-operative period more difficult.
FUE has been controversial since its introduction in 2000. The controversy surrounding FUE centers on the success rate and results of FUT, how many FUE sessions are needed, the marketing of FUE, and the rise of FUE clinics that do not have doctors.
The data available on FUE and FUT growth rates are not very extensive. We have limited data, and it shows a wide range of growth rates, from a difference of 24.6% between FUE (Beehner 2016) to almost no difference (Josephitis & Shapiro 2018), when done in small sessions and in a thorough manner. However, this data shows that FUT harvesting has more variability than FUE. Most physicians who do both FUT or FUE find FUT more consistent. Both procedures are preferred for smaller surgeries. FUE can have serious effects on the donor area if performed at “mega sessions”. Because grafts are removed individually, this causes a thinning effect within the donor. A donor may experience a generalized thinning effect, or “blown out” patches, if too many grafts have been removed simultaneously. Most doctors recommend starting with FUT first and moving on to FUE later. However, opinions differ. However, the most important issue in FUE is the current wave of aggressive online marketing, and subsequent proliferation of non-doctor FUE centers. Many large medical device manufacturers have created “turn-key” FUE systems. They now sell these protocols and devices to non-hair transplant physicians looking to increase their revenue. The companies claim that the device allows them seamlessly to perform delicate and precise procedures without needing any prior experience. They even offer to send technicians if they are not comfortable or don’t want to do the surgery themselves – which is a highly illegal practice in America. In certain countries, this shift to technician-run FUE and profit-driven FUE has led to the creation of clinics in which FUE is 100% performed by technicians. These clinics have a doctor who will see the patient every morning and make some markings before turning the case over to technicians. The technicians will tell the patient how many grafts they should remove and where to place them. All medical and surgical decisions are made without any legal or moral responsibility. This model is becoming more popular than expected, resulting in serious complications and disastrous outcomes for patients. This model should not be used for FUE. Patients should look for a team that is experienced in FUT and FUE, with a protocol and dedicated clinic. They also need to have a track record of performing high-quality FUE.
References
Beehner, M.L. (2016). FUE vs. FUT-MD: Study of 1,780 Follicles in Four Patients. Hair Transplant Forum
International. 2016; 26(4): 160-161
Josephitis, D., Shapiro, R. (2018). FUT vs. FUE Graft Survival: A Side-by-Side Comparison of Three
Patients Undergoing a Routine 2,000+ Graft Hair Transplantation. Hair Transplant Forum
International. 2018; 28(5): 179-182